Introduction: Psoriasis is a chronic inflammatory skin disease characterized by raised, red, scaly patches (plaques) that can be itchy and uncomfortable.

Traditional treatments include topical steroids, systemic medications, and phototherapy with ultraviolet light. In recent years, red light therapy (RLT) has drawn interest as a potential therapy for psoriasis that avoids UV exposure. Fans of RLT – including biohackers and holistic wellness advocates – suggest it can soothe psoriasis by reducing inflammation and promoting skin repair. This comprehensive guide explores how red (and near-infrared) light may benefit psoriasis, reviews the latest scientific evidence and expert opinions, and offers tips on choosing effective at-home or professional red light therapy options for managing psoriatic plaques.
How Red Light Therapy Affects Psoriasis
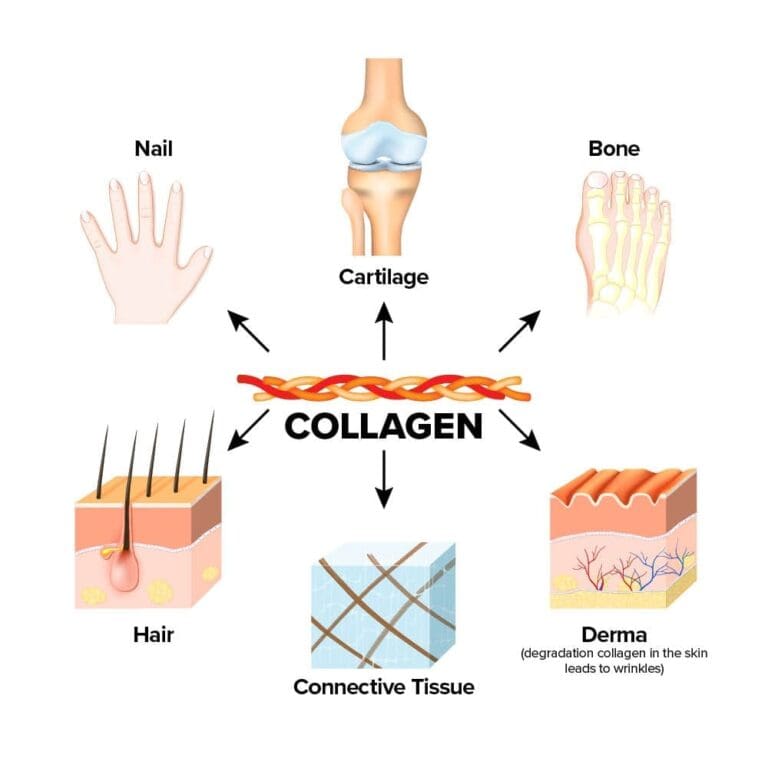
Psoriasis is driven by an overactive immune response in the skin, leading to rapid turnover of skin cells and inflammation. Red light therapy, also known as photobiomodulation, is thought to help by modulating the immune and inflammatory processes underlying psoriasis. Red light (typically in the 630–660 nm range) and near-infrared light (800–880 nm) penetrate into the dermis where psoriasis inflammation resides, influencing various cell types – including keratinocytes, T-cells, and dendritic cells – to encourage a healthier, more normal skin function.
Essentially, RLT emits photons that are absorbed by cellular chromophores (like mitochondria), boosting cellular energy production and releasing signals that can reduce pro-inflammatory cytokines while increasing tissue repair activity.
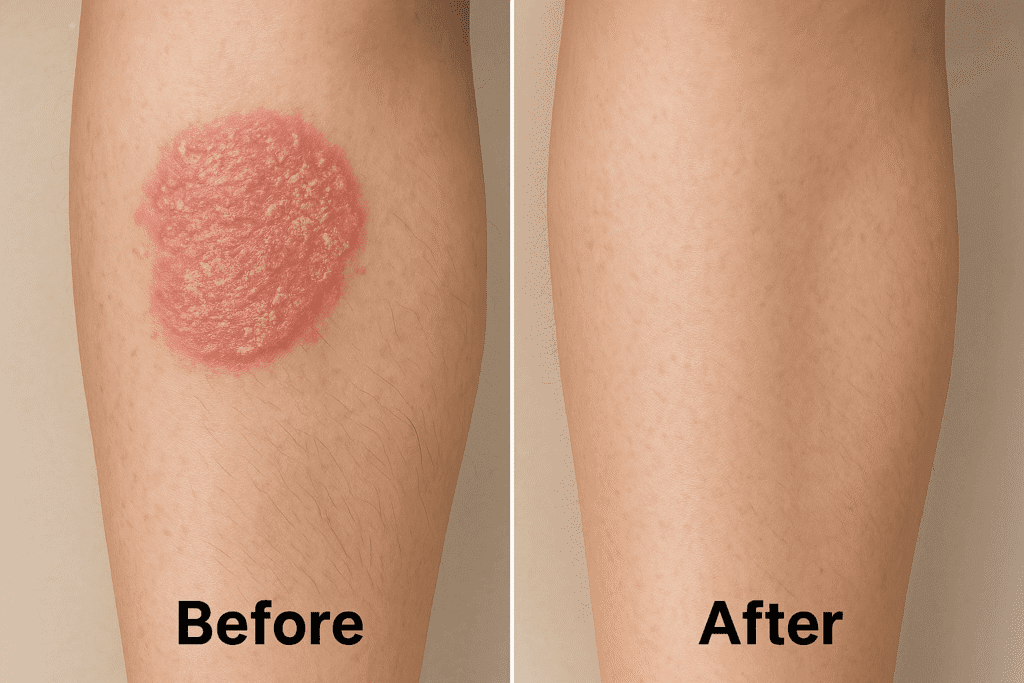
Early research and clinical reports support the idea that low-level light therapy can improve psoriatic lesions. Unlike UV phototherapy (such as NB-UVB) which works by suppressing skin cell growth through a controlled damage mechanism, red light produces no ionizing radiation or sunburn. Instead, it exerts a gentler influence: studies have shown that red and near-infrared light can reduce the thickness and redness of psoriasis plaques by curbing inflammation. For example, red/NIR light has been observed to down-regulate inflammatory markers (like IL-6 and TNF-alpha) in psoriatic skin, and to promote regeneration of healthy skin cells. One clinical trial investigated a combination of 633 nm red and 830 nm near-infrared LED therapy on recalcitrant psoriasis and found a notable reduction in lesions, attributed to the anti-inflammatory effects of those wavelengths. Patients in that study experienced less scaling and thinner plaques after a series of treatments, without the burning or UV damage risk associated with conventional phototherapy.
It’s important to note that psoriasis has multiple subtypes and severities, and RLT may be more suitable for some cases than others. Plaque psoriasis (the most common form) has been the main focus for light therapy. Red light’s ability to calm inflammation and potentially slow abnormal cell growth directly addresses two key aspects of plaque psoriasis. Additionally, red light may help relieve the persistent itch and discomfort by reducing the local inflammatory signals in the skin. Another potential benefit is improved skin barrier function – psoriasis lesions often have broken, dry skin; by stimulating collagen production and blood circulation, RLT could support barrier repair and reduce cracking. Unlike UVB therapy which intentionally causes minor skin injury to trigger improvement, RLT aims to assist the skin’s own healing processes in a non-damaging way. This difference means RLT can be used more frequently (even daily) without cumulative harm, though it also might yield slower or subtler results than aggressive UV therapy. Overall, the biological rationale for using red light in psoriasis is strong: it targets inflammation and promotes tissue normalization, aligning well with the needs of psoriatic skin.
Scientific Evidence and Expert Insights
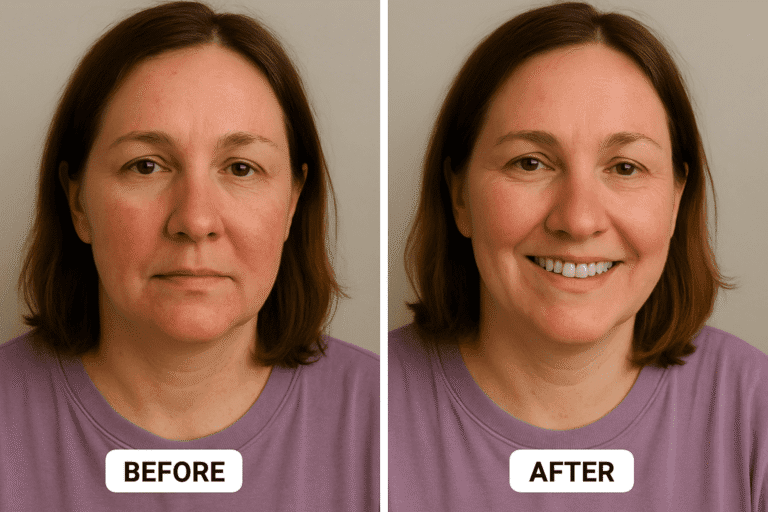
Is there proof that red light therapy actually works for psoriasis? Emerging studies and case reports indicate positive outcomes, though large-scale trials are still limited. One oft-cited preliminary study (Ablon et al., 2010) treated nine patients with stubborn plaque psoriasis using a combination of 830 nm and 633 nm LED light. After about a month of twice-weekly sessions, all patients showed improvement, with clearance of plaques ranging from 60% up to 100% in the treated areas.

Patient satisfaction was very high, and there were no adverse effects. This small study suggested that even psoriasis that hadn’t responded to other treatments could substantially improve with red/NIR light therapy.
Another clinical trial compared red light therapy against a standard psoriasis treatment. Patients using a 630 nm red LED device at home daily for 4 weeks saw significant reductions in their Psoriasis Area and Severity Index (PASI) scores, although in that particular study the red light’s improvement was not quite superior to narrowband UVB therapy. In other words, UVB phototherapy remains a gold standard (with ~70% of patients achieving PASI-75 clearance in some analyses), but red light may offer an alternative for those who can’t use UVB or want an adjunct to lower their inflammation. A 2023 comprehensive review on light-based treatments noted that red light (620–770 nm) and blue light (400–480 nm) have both shown efficacy in plaque psoriasis, and lists them as emerging third-line phototherapy options for managing the disease. Blue light has a more shallow penetration but can reduce keratinocyte proliferation, while red/NIR penetrates deeper to affect immune cells; both can safely improve plaques according to the review.
Dermatology experts remain cautiously optimistic. Psoriasis is notoriously variable, and not every patient will respond the same way to RLT. The National Psoriasis Foundation recognizes that low-level laser or light therapies have been used with some success in small studies, but they’re not yet mainstream. One reason is that results, while positive, have been inconsistent across different trials. For instance, a study combining topical curcumin (a natural anti-inflammatory) with red light showed added improvements in psoriasis lesions by modulating molecular pathways like NF-κB. This hints that RLT could be part of a multi-modal approach. On the other hand, some trials did not find red light alone to outperform placebo significantly – possibly due to differences in light dose, duration, or psoriasis severity.
Clinicians do agree on one thing: red light therapy for psoriasis appears extremely safe and well-tolerated. Unlike some systemic drugs that suppress the immune system body-wide, RLT’s effects are localized to the skin and carry no risk of liver or kidney damage. Patients treated with red light have reported no pain (it’s a painless procedure) and no serious side effects, aside from maybe mild warmth or temporary redness. This safety profile makes it an attractive option for patients seeking more natural or adjunct treatments. According to a clinical review, low-level light therapy “has been widely applied in dermatology” and is now considered a potentially effective method for psoriasis, albeit currently as a third-line or supplemental therapy. The review specifically noted that the combination of 633 nm red + 830 nm near-IR LEDs showed promise in treating recalcitrant psoriasis that didn’t respond to other methods. This combination likely works by harnessing the benefits of both wavelengths – red for superficial inflammation and near-IR for deeper immune modulation.
In summary, the evidence to date suggests that red light therapy can reduce psoriasis symptom severity, especially plaque thickness and redness, and possibly extend remission times, all with minimal downsides. While it may not replace primary treatments for moderate-to-severe cases, it provides a novel approach that patients can use in conjunction with topical agents or between doctor’s visits. More robust clinical trials are underway or needed, but dermatologists are already exploring RLT as part of personalized psoriasis care for patients seeking alternatives. As one set of authors concluded, low-level light therapy holds “promising expectation” for psoriasis management in the future.
At-Home vs. Professional Red Light Therapy for Psoriasis
If you’re considering red light therapy for psoriasis, you have options ranging from clinic-based treatments to at-home devices. Each approach has its pros and cons:
- In-Clinic Treatments: Dermatologists or phototherapy centers may offer red light therapy sessions, although it’s less common than UV phototherapy. Some clinics have whole-body light therapy units (essentially booths lined with LEDs) or large panels that can be positioned over affected areas. The advantage of professional treatment is expert oversight – the staff can ensure the correct dose and track improvements. Clinics may also have higher-powered machines, meaning potentially shorter sessions or greater light penetration. Additionally, clinics might combine red light with other therapies: for example, doing an infrared light session after an excimer laser treatment (excimer is a targeted UVB laser for psoriasis) to reduce post-treatment inflammation. However, RLT is not yet a standard offering at every dermatology office for psoriasis. UVB phototherapy remains more prevalent and is often covered by insurance for psoriasis, whereas red light therapy might be considered experimental and not covered. If you do find a provider, expect to need multiple sessions per week initially – similar to UV therapy schedules – which could be a time commitment. The in-clinic route may be ideal if you have widespread psoriasis (covering large body areas) where a full-body professional unit can treat you more efficiently than a small home device. It’s also a good choice if you want the guidance of healthcare professionals to monitor your skin’s response.
- At-Home Devices: Given the chronic nature of psoriasis, many sufferers are interested in home light therapy that can be done conveniently and continuously. Indeed, there are at-home red light therapy panels, lamps, and even wearable wraps that users deploy on psoriatic patches. The benefit here is convenience and consistency – you can do short daily sessions without driving to a clinic. It also gives a sense of control; you can adjust frequency based on how your skin is doing. Home devices for psoriasis should ideally be larger panels or mats, since plaques often cover areas like the elbows, knees, or back. For example, an individual with psoriasis on their legs might use a sizable LED panel (say 2 feet by 1 foot) to bathe the plaques in red light all at once, rather than spot-treating small sections. Some people even use full-body red light beds (these look like tanning beds but with red LEDs) as part of their home routine, which can address multiple lesions simultaneously. Of course, these larger devices can be expensive. Smaller handheld red light devices (like those sold for general skin improvement) can also be used on psoriasis, but it would require treating one patch at a time for several minutes each, which might be tedious if you have many lesions.
When using at-home RLT for psoriasis, it’s critical to follow guidelines: protect your eyes (especially if the device emits any blue light or is very bright – use goggles as provided), and avoid using it on areas where you have open wounds or severe cracking without medical advice. Also, be mindful of any photosensitizing medications you might be on; although red light isn’t UV, certain drugs could in theory make you more sensitive to light of any kind. The great news is that home devices for psoriasis have shown positive results in studies: one trial of a home-use LED panel (emitting both red and blue light) reported significant plaque improvements after daily use, and patients found it easy to use and gentle on the skin. This suggests that self-treatment is feasible for disciplined patients.
- Hybrid Approaches: Some psoriasis patients might use a hybrid approach: getting periodic in-office treatments (such as powerful light therapy or other procedures for stubborn plaques) and doing maintenance with red light at home. For example, after achieving clearance with NB-UVB phototherapy or biologic drugs, a patient might use red light on any small emerging spots to help keep them in check. Because RLT can be done safely long-term, it could help prolong remission periods between flare-ups. Always communicate with your dermatologist about your at-home therapies – they can help track how it’s working and ensure it complements your medical regimen.
Selecting a Red Light Therapy Device for Psoriasis (Buyer’s Guide)
Choosing the right RLT device for psoriasis comes down to matching the device’s capabilities with your specific condition. Here are key considerations:
- Treatment Coverage: Psoriasis plaques can range from small coin-sized spots to large patches covering knees, elbows, scalp, etc. For extensive psoriasis, larger panel devices or light therapy lamps will save time. These let you treat a broad area in one sitting. On the other hand, if you only have a few localized plaques (say on the ankles or one elbow), a smaller targeted device might suffice. There are even handheld laser devices (low-level lasers) that emit 630 nm red light in a concentrated beam, which could be used for isolated stubborn plaques or thick lesions (some users apply these to particularly scaly spots to try to thin them out). Evaluate the size of the light array – bigger panels (with more LEDs) will generally deliver more uniform coverage for even improvement across the plaque.
- Wavelength and Light Type: For psoriasis, look for devices that emit red light in the mid-600 nm range and/or near-infrared light around 800 nm. Many quality panels include a mix of 660 nm and 850 nm LEDs. The 660 nm is visible red that helps surface skin inflammation, while 850 nm (invisible NIR) penetrates deeper to joints and tissues – potentially helpful if you have psoriatic arthritis-related stiffness in addition to skin symptoms. Some devices also incorporate blue light (around 415–420 nm), which recent studies have found can reduce the hyper-proliferation of keratinocytes and even safely improve plaque psoriasis in certain cases. Blue light only reaches shallow skin layers, so it could be an extra tool for surface scaling and bacteria in plaques, while red goes deeper. Overall, a dual or tri-wavelength device might offer comprehensive benefits. Ensure any device you consider clearly lists its wavelengths and that those match known therapeutic ranges for skin.
- Power and Dose: Check the device’s power output (irradiance) and recommended treatment time. Psoriasis plaques often are thicker skin, so to get light penetration, you need sufficient dose. Many clinical studies on psoriasis used devices delivering around 100 mW/cm² or more, with session doses on the order of 10–50 J/cm². At home, this might translate to, for example, a 15-minute session at 6 inches distance for a mid-powered panel. Some home devices publish their irradiance (e.g., 100 mW/cm² at 6 inches). If not, look for user feedback on effectiveness. Adjustability is a nice feature: certain devices let you choose only red, only NIR, or both, and adjust intensity. For beginners, starting with a moderate intensity and shorter sessions, then ramping up as needed, is a prudent strategy to avoid any skin irritation.
- Ergonomics and Ease of Use: Because you may need to use this device frequently, practical design matters. Panel devices often come with stands or door hooks so you can stand/sit in front of them. Some have adjustable angles to better target legs vs. torso. If you have psoriasis on hard-to-reach areas (like your lower back), consider how you’ll position the device – a panel on a stand could be angled, or a smaller device might need someone’s help to hold it. Wearable wrap-style LED devices are a newer option: these are flexible pads embedded with LEDs that strap onto an area (for instance, you could wrap one around your arm or leg). They allow you to move around during treatment. Just ensure any wearable has sufficient coverage for your plaques. Additionally, if you plan to treat while doing something (like watching TV), devices with automatic timers and shutoff are useful so you don’t have to clock-watch. Simplicity in controls (one-button operation) can make sticking to routine easier.
- Safety Features: Verify that the device is certified or cleared for safe home use. Eye safety is critical; many panels come with goggles – use them. Devices should not get excessively hot; good designs have cooling fans or heat sinks to dissipate heat from the LEDs. If you have sensitive skin or a history of photosensitivity, consider devices that allow lower intensity settings to start. Also, research if the device has been tested specifically on psoriasis or sensitive skin conditions. Some manufacturers may provide white papers or customer case studies on psoriasis use – those can be reassuring.
- Reviews and Reputation: Since the home light therapy market is growing, stick with reputable brands that have positive reviews from users with psoriasis or similar conditions. Reading testimonials or community forums (e.g., psoriasis support groups discussing RLT) can provide insight into which products delivered real relief. Avoid cheaply made gadgets with little information on specs – if it’s not delivering the right wavelength or enough power, it may be a waste of time. It’s worth investing in a quality device that you’ll use for the long term, as psoriasis is an ongoing condition.
Using Red Light Therapy for Psoriasis – Tips for Success
To get the most out of red light sessions and manage your psoriasis safely, keep in mind these tips and best practices:
- Consistency and Patience: As with most psoriasis treatments, consistency is key. You may need to use red light therapy regularly for several weeks before seeing significant changes in your plaques. Set up a routine – for example, 10-15 minutes of light therapy every evening on affected areas. Some people do it while listening to a podcast or incorporate it into their meditation/relaxation time. Track your lesions’ appearance bi-weekly with photos; improvements might include reduced redness, thinner scales, or smaller diameter of plaques. Celebrate small progress – reduced itching or slightly less scale is a win that indicates it’s working and will compound over time.
- Pre-Treatment Skin Prep: Make sure the psoriasis plaques are clean before treatment. Gently remove any heavy creams or occlusive ointments (if you use them) because those could block light penetration. It may also help to soften thick scale beforehand – for instance, taking a warm shower or using a keratolytic salicylic acid lotion to remove excess scale (if recommended by your doctor). Less scaling means the light can penetrate more uniformly into the lesion. However, avoid causing irritation by over-scrubbing. Light therapy can be done on fully dry skin; there’s no need to apply anything special on the skin for RLT (unlike PDT which requires a photosensitizer).
- Don’t Replace Doctor-Prescribed Treatments Abruptly: If you are on medications (like methotrexate, biologics, or topical steroids), consult your dermatologist before making changes. Red light therapy can often be added to your regimen without issue – it may even help you eventually reduce reliance on some meds, but that should be done under guidance. Many patients use RLT as an adjunct: for example, continuing their low-dose topical steroid twice a week and doing red light on other days to keep inflammation down. Over time, some find they can maintain with just light therapy and moisturizers, but individual results vary. It’s a balance between exploring new treatments and not risking a severe flare by quitting something that’s working.
- Watch for Improvements and Flares: Interestingly, a minority of patients might experience a temporary flare or irritation when starting light therapy (perhaps due to increased immune activity as skin cells respond to light). If you notice any new redness or your psoriasis seems to worsen initially, don’t panic – reduce the session length or take a short break and then resume more slowly. Often, the skin adapts. Conversely, you might notice rapid improvements in some lesions and not others. It’s possible that thinner or newer plaques respond faster than very old thick plaques. Focus the light on the stubborn areas a bit longer, if needed, and be diligent. If a plaque fully clears, continue treating that area a couple of times weekly to suppress it from rebounding.
- Holistic Skin Care: Red light therapy works best in conjunction with general skincare for psoriasis. Keep your skin well-moisturized – apply a fragrance-free, thick moisturizer or emollient after RLT sessions to lock in moisture (the light may enhance absorption of products applied afterward, which can be beneficial for hydration). Address triggers that worsen your psoriasis: stress, smoking, alcohol, and certain foods can cause flares. While RLT can reduce the inflammation, you’ll have even better results if you minimize triggering factors in parallel. Some patients also find that combining light therapy with gentle exfoliation (like using a tar shampoo for scalp plaques or urea creams on thick scale) helps the process. Just be careful not to irritate the skin; always err on the side of gentle care since the goal is to calm the immune response.
- Sun Exposure Considerations: One advantage of red light is that it doesn’t have the risks of UV. You can use RLT year-round, whereas doctors often limit UV phototherapy cumulative dosing to prevent skin aging or cancer risk. However, continue to protect your skin from natural sunburn – a bad sunburn can trigger the Koebner phenomenon in psoriasis (where new lesions appear at sites of skin injury). So, sunscreen on exposed skin is still important outdoors. Red light therapy itself won’t make you photosensitive like some medications do, but if you’re on a drug like acitretin (which can increase sun sensitivity), take normal sun precautions.
- Manage Expectations for Severity: For mild to moderate plaque psoriasis, red light therapy might alone bring significant relief and visible clearance. For severe cases (covering large body percentages or with very thick plaques), you may still require conventional systemic treatments for adequate control, using RLT as a supplementary measure for symptom relief. The nice thing is, even if you need to remain on meds like biologics, adding red light poses no known conflict and might further improve your skin’s texture and resilience. Think of RLT as a useful tool in the toolbox – very safe, moderately effective on its own, and potentially synergistic with other therapies.
Conclusion
Living with psoriasis is a journey of managing flare-ups and finding therapies that keep the condition in check while maintaining quality of life. Red light therapy represents a cutting-edge yet accessible approach that aligns with the needs of many psoriasis patients: it’s non-invasive, drug-free, and focused on reducing the inflammation that drives psoriatic lesions. The latest research and user experiences indicate that RLT can lead to calmer skin – plaques that are less red, less scaly, and less bothersome. While it’s not a silver bullet or a definitive cure (psoriasis is a complex systemic condition, after all), red light therapy offers a promising adjunct or alternative for those seeking relief beyond creams and injections.
From small pilot studies showing impressive clearance rates to dermatologist reviews highlighting low-level light as a viable therapy, the evidence base for RLT in psoriasis is building. We also have decades of experience using light (in the form of UV) for psoriasis, so the concept of phototherapy is well-grounded – red light simply provides a safer spectrum to work with long-term. Many psoriasis sufferers have already embraced at-home red light panels as part of their daily routine and report smoother, happier skin and a reduction in flare frequency.
In the spirit of holistic self-care, red light therapy empowers patients to take an active role in soothing their skin. It can be particularly appealing for those sensitive to medication side effects or those who’ve hit plateaus with other treatments. And even beyond psoriasis plaques, RLT may confer side benefits like improved mood (some studies suggest bright light can uplift mood, relevant since psoriasis flares are often stress-related) and better sleep regulation – making it an attractive wellness practice overall.
In conclusion, red light therapy is shining new hope on psoriasis management. By harnessing the gentle power of light to dial down inflammation and boost skin repair, it helps restore a measure of balance to overactive skin. If you’re a psoriasis patient, consider discussing RLT with your healthcare provider as a complementary option. With realistic expectations and consistent use, you might find that a daily dose of red light becomes a bright spot in your regimen, leading you toward clearer skin and a better quality of life.
🔗 Resources & References
Clinical Research & Reviews
- American Academy of Dermatology – Psoriasis Treatment Guidelines
- Ablon G. Combination 830 nm and 633 nm LED Treatment of Recalcitrant Psoriasis: A Case Series. Clinical, Cosmetic and Investigational Dermatology, 2010. Link to article
- Huang Y-Y, Sharma SK, Carroll J, Hamblin MR. Biphasic dose response in low level light therapy – An update. Dose-Response. 2011. Read study
- Barolet D, Boucher A. Prophylactic low-level light therapy for the treatment of hypertrophic scars and keloids: A case series. Lasers in Surgery and Medicine. Wiley Online Library
Medical & Institutional Guidance
- National Psoriasis Foundation – Light Therapy
- Cleveland Clinic – Phototherapy for Psoriasis
- Mayo Clinic – Psoriasis Treatment Options
Expert Commentary & Real-World Use
- DermNet NZ – Psoriasis and Phototherapy
- Harvard Health Publishing – Can red light therapy ease skin conditions like psoriasis?
Patient Support & Further Reading